Abstract
Introduction: There are many etiologies for thrombocytopenia, such as viral suppression, disseminated intravascular hemolysis, and immune thrombocytopenic purpura (ITP). Zika virus (ZIKV) recently emerged in the Americas and was first detected in Puerto Rico in late 2015. ZIKV disease is generally mild; however, it has been infrequently associated with life-threatening outcomes including severe thrombocytopenia. We sought to define incidence and outcomes of ZIKV disease patients with thrombocytopenia.
Methods: We reviewed the medical records of patients with reported thrombocytopenia (platelet count ≤ 100,000 cells/µL) among patients with ZIKV disease (defined by detection of ZIKV nucleic acid by RT-PCR or anti-ZIKV IgM antibody by ELISA and the presence of symptoms) that had been reported via passive surveillance. Among patients with confirmed thrombocytopenia, we collected data on medical history, interventions, and patient outcomes. Cases of severe thrombocytopenia were defined by: a) platelet count <20,000 cells/µL; or b) platelet count <50,000 cells/µL with a clinical diagnosis of and treatment for ITP. Cases in which another likely cause of thrombocytopenia was identified (e.g., sepsis, immunosuppression) were excluded from analysis. Data were collected in REDCap®.
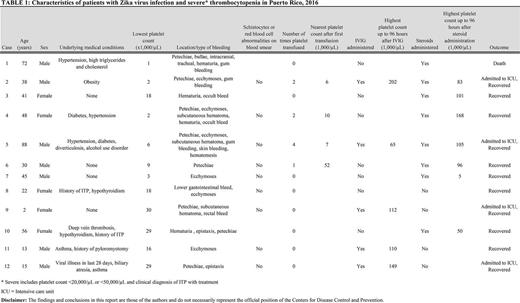
Results: Of 37,878 patients with ZIKV disease reported during 2016, a total of 436 had reported thrombocytopenia. Among patients with medical records available for review, 48 (0.1%) had confirmed thrombocytopenia in the absence of an identified etiology. Twelve of these 48 patients (25%) had severe thrombocytopenia (Table 1), and 36 (75%) had non-severe thrombocytopenia.
Median age of patients with severe and non-severe thrombocytopenia was 39.5 years (range: 2-88) and 49 years (range: 1-88 years), respectively; 7 (58%) and 19 (53%) were male. Two (17%) patients with severe and 3 (8%) with non-severe thrombocytopenia had a history of ITP. All patients reported recent illness, which most frequently included rash (73%) and/or fever (77%). Median nadir platelet count of patients with severe and non-severe thrombocytopenia was 12,500 cells/µL (range: 1,000-30,250) and 70,000 cells/µL (range: 24,000-100,000), respectively, which occurred a median of 5.7 days (range: 1.4-15.6) and 4.5 days (range: 0.4-34.1) after symptom onset. Blood smears were performed in 9 (75%) patients with severe and 18 (50%) with non-severe thrombocytopenia. No patients with severe thrombocytopenia and 1 (2.8%) patient with non-severe thrombocytopenia had fragmented red blood cells; visualization of platelets on smear was consistent with low platelet counts. Whereas 11 (30.6%) patients with non-severe thrombocytopenia had petechiae, hematuria, or gingival bleeding, all (100%) patients with severe thrombocytopenia had hemorrhagic manifestations including petechiae (66.7%), hematuria (33.3%), ecchymoses (50%), gastrointestinal bleeding (25%), or intracranial hemorrhage (8.3%). Only patients with severe thrombocytopenia were diagnosed with ITP. Only patients with severe thrombocytopenia received platelet transfusion (n = 4; 33.3%) and/or intravenous immunoglobulin (IVIG) (n = 5; 41.7%). The patients with severe thrombocytopenia that received IVIG all had an up-trending platelet count after IVIG administration. Eight (66.6%) patients with severe thrombocytopenia and 9 (25.0%) with non-severe thrombocytopenia received steroids. Among those who received platelet transfusions, the median platelet count increase following transfusion was 6,000 cells/µL; 25% had a decreased platelet count following transfusion. Outcomes among patients with severe or non-severe thrombocytopenia included hospitalization (100% vs. 53%), admission to the intensive care unit (33% vs. 0%), and death (8.3% vs. 0%).
Conclusions: Thrombocytopenia appears to be an uncommon occurrence in patients with ZIKV infection. Though rare, severe thrombocytopenia associated with ZIKV disease can be fatal; treatment is necessary. Platelet transfusions alone may not be effective, whereas administration of corticosteroids and IVIG may be of benefit in some cases. Further study is needed to characterize the pathogenesis of ZIKV-associated severe thrombocytopenia and interventions associated with survival. Appropriate diagnosis of the underlying etiology of thrombocytopenia is time-sensitive and crucial to improving patient outcome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal